Health News
blood-brain barrier, brain inflammation, cognitive behavior, cytokines, gut microbiota, gut-brain axis, immune response, immune system, indole-3-lactic acid, intestinal barrier, intestinal inflammation, lactobacillus, lactobacillus transplantation, neuronal apoptosis, parasite infection, parasite pathology, toxoplasma gondii, toxoplasma infection, toxoplasmosis, toxoplasmosis treatment
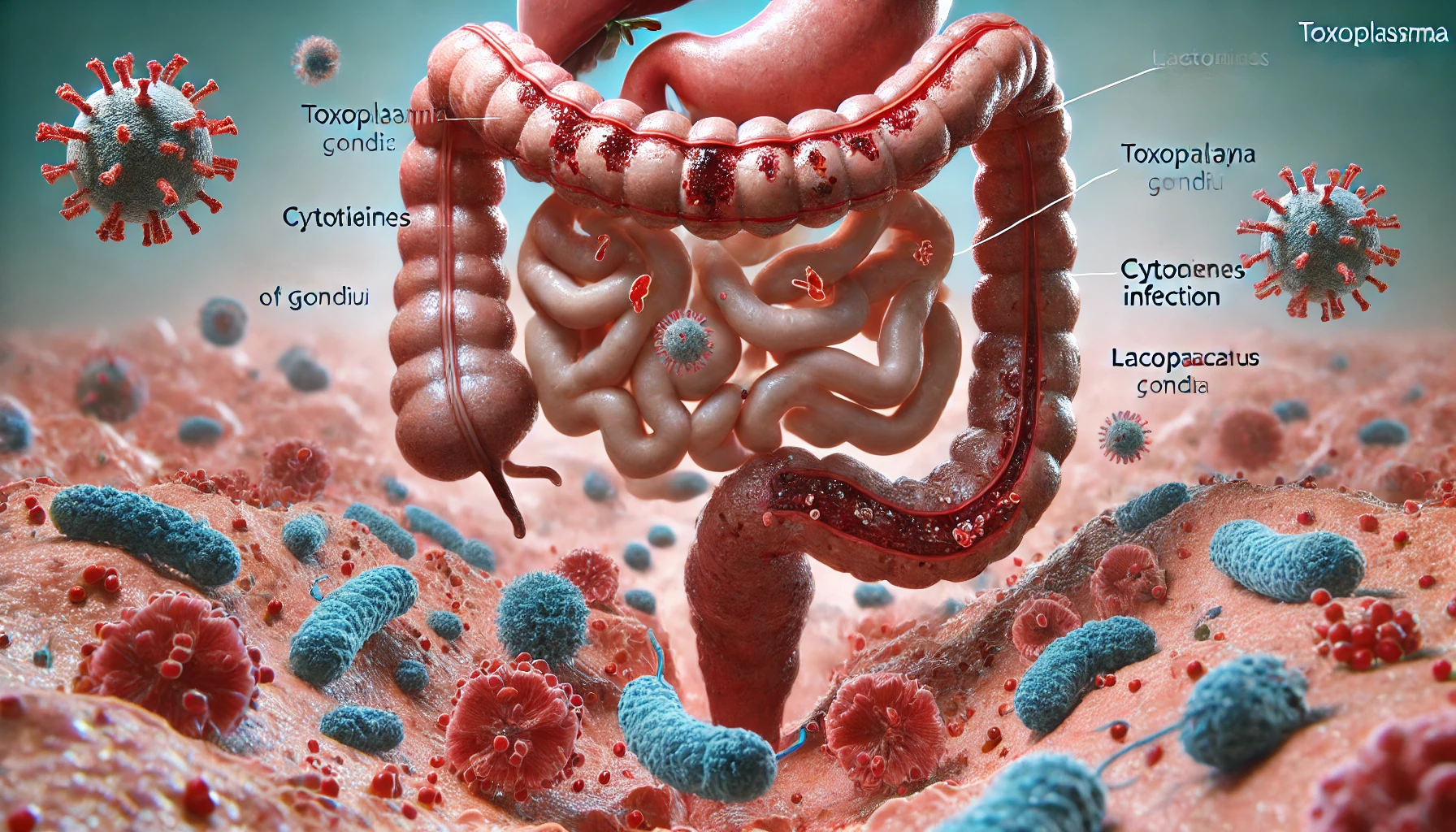
Immune Response and Gut Microbiota: How Toxoplasma gondii Infection Triggers Pathology
The interaction between the immune response and the gut microbiota plays a pivotal role in the pathology caused by Toxoplasma gondii infection. Studies have revealed that inflammation in the intestinal epithelium, triggered by the body’s immune system, exacerbates the infection’s effects and alters the diversity of gut bacteria. Reintroducing key bacterial species has been found to alleviate this parasite-associated pathology.
Understanding Toxoplasma gondii
Toxoplasma gondii is a protozoan parasite capable of infecting nearly all warm-blooded animals, including humans. This parasite can only reproduce sexually within members of the cat family; however, other animals, such as mammals and birds, act as intermediate hosts. Once infected, these hosts carry the parasite, which can spread through the environment.
When an infected cat excretes long-lived oocysts in its feces, these oocysts can be ingested by intermediate hosts. Inside the host’s intestines, the cysts break down, allowing the parasites to invade epithelial cells and transform into a rapidly multiplying form. This leads to intestinal infection, characterized by inflammation and a subsequent alteration in the gut microbiota.
The Spread of the Parasite in the Body
Following the breakdown of the intestinal barrier, Toxoplasma gondii parasites are released and spread throughout the host’s body. They invade tissues, particularly in the brain, eyes, and muscles, converting into semi-dormant cysts that can remain for years. In humans, T. gondii infections are widespread, with some regions reporting infection rates exceeding 50% of the population.
Most people infected with T. gondii do not show symptoms, but in some cases, the parasite can breach the blood-brain barrier and cause neural apoptosis, which may lead to the neurological disorders associated with toxoplasmosis.
The Role of Immune Response in T. gondii Infection
Intestinal inflammation plays a key role in the body’s defense against T. gondii, as it helps to suppress parasite reproduction. However, this immune response also disrupts the balance of the gut microbiome, which may have implications for the gut-brain axis. The production of cytokines by immune cells is crucial for controlling the infection, but it also has a significant impact on the gut ecosystem.
Gut Bacteria’s Role in Mitigating Inflammation
Recent studies, particularly those conducted at Yunnan Agricultural University in China, have identified bacterial metabolites that reduce the severity of intestinal inflammation caused by T. gondii. The research highlights how certain gut bacteria, when preserved or replenished, can mitigate damage to the gut microbiome during infection.
A team from Southern Medical University in China further investigated this by comparing the gut microbiota and cognitive behavior in two groups of mice—those with a functional immune system and those without. The results shed light on the connection between the gut microbiome and brain health in the context of T. gondii infection.
Studying the Effects of T. gondii on Gut and Brain Health
The researchers used pathogen-free wild-type (WT) mice with functional immune systems and vimentin gene knockout (vim−/−) mice, which are immunocompromised. The mice were orally infected with varying doses of T. gondii cysts or left uninfected as controls. Three months post-infection, the mice were subjected to various behavioral tests, including swimming tests, maze navigation, and open-field tests to measure learning, memory, anxiety, and sociability.
Results showed that T. gondii infection caused a marked decline in learning and memory abilities, particularly in WT mice. Additionally, these infected mice exhibited depression-like symptoms and reduced anxiety levels. Interestingly, the immunocompromised mice showed fewer cognitive deficits than the WT group.
Impact of T. gondii on Brain Tissue
After the behavioral tests, the researchers examined the brains of the mice for the presence of T. gondii cysts. The results showed a significantly higher cyst load in the WT mice compared to the immunocompromised mice. Further transcriptome sequencing of brain tissue revealed an upregulation of apoptosis-related genes in the WT mice, confirmed by immunofluorescence staining.
This raised questions about whether the previously reported loss of gut bacteria played a role in the observed brain pathology. Researchers then analyzed the gut microbiota of infected and uninfected mice to see if differences in species richness might explain the cognitive effects.
Changes in Gut Microbiota During Infection
Using fecal samples from the mice, researchers compared the gut microbiota composition of infected and uninfected mice. They found that while the species richness in the immunocompromised mice remained stable, the WT mice experienced a significant reduction in gut bacteria. This included a loss of Lactobacillus species, which are known to regulate the immune system and maintain gut epithelial integrity.
Restoring Gut Microbiota to Reduce Pathology
In an effort to restore the balance of gut bacteria, the researchers introduced two species of Lactobacillus into the WT mice through gavage. The results were promising: the reintroduction of these bacterial species significantly improved the survival rates of infected mice and decreased the parasite load in their brains. Additionally, the damage to the intestinal barrier and brain tissue, as well as neuronal apoptosis, was greatly reduced.
The researchers attributed this improvement to an increase in CT8+T cells and the production of IFN-γ—important components of the immune response. These elements are indirectly activated by Lactobacillus-related metabolites, particularly indole-3-lactic acid (ILA), a compound that is reduced during T. gondii infections.
The Therapeutic Potential of Gut Bacteria
The findings of this comprehensive study suggest that the immune system’s response to Toxoplasma gondii exacerbates the pathology of the infection. In WT mice, the immune response was more aggressive, leading to greater damage to the gut microbiota and subsequently affecting brain health. However, when key bacterial species like Lactobacillus were restored, the pathology was mitigated, highlighting the role of gut bacteria in maintaining both gut and brain health.
One of the key metabolites, ILA, which is downregulated during infection, has shown potential as a therapeutic compound. If researchers can find a way to deliver ILA effectively, it could provide an easier treatment option for T. gondii infections compared to bacterial transplantation.
Conclusion
In summary, Toxoplasma gondii infection triggers a complex immune response that not only targets the parasite but also disrupts the gut microbiota and damages the intestinal barrier. This disruption has a ripple effect, leading to brain inflammation and neuronal apoptosis, which can manifest as cognitive and behavioral disorders. However, the restoration of beneficial gut bacteria, particularly Lactobacillus, offers hope for reducing the damage caused by the infection.
Future research may focus on harnessing bacterial metabolites like indole-3-lactic acid as therapeutic agents to treat toxoplasmosis, providing a more efficient alternative to direct bacterial transplantation. Understanding the interaction between the immune system, gut microbiota, and Toxoplasma gondii will be key to developing more effective treatments for this widespread parasitic infection.